Gynaecologic 2D/3D Ultrasound Examination
A gynaecologic ultrasound examination is a non-invasive screening test to evaluate a woman’s reproductive system. Thanks to the use of ultrasonic waves generated by advanced ultrasound devices, and the use of state-of-the-art technical solutions in the software of the device, it is possible to obtain very precise images of individual structures.
A gynaecological ultrasound examination aims to assess the following:
- uterine walls – including the uterus (detection of developmental defects of the uterus), the presence of pathological structures (myoma/adenomyosis lesions, tumours);
- endometrium – its condition and the presence of endometrial polyps, endometrial hyperplasia, endometrial cancer, as well as assessment of the endometrial function (for hormone disorders, cycle monitoring)
- ovaries – assessment of the structure (presence of tumours, cysts) and ovarian function (follicular apparatus, presence of ovarian follicle), and evaluation of ovarian stimulation for IVF needs
- fallopian tubes – proper functioning fallopian tubes cannot be examined by the ultrasound test, but diagnostics of their pathology is possible, such as the oviduct hydrocephalus, ectopic pregnancy, and ovarian cysts
- The Douglas cavity – exclusion/confirmation of the presence of fluid in the cavity, as well as pathologies (tumours, endometriosis)
The gynaecologic ultrasound is most often performed with a transvaginal probe (in sexually active patients), while in other cases it may be performed using an abdominal or rectal probe.
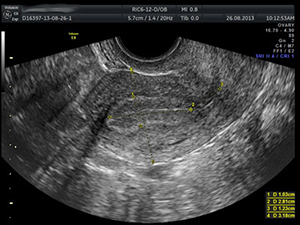
The use of 3D ultrasound technology has made it possible to circumvent many of the limitations of 2D projection. 3D technology allows you to save a very large series of sequential ultrasound images into a volumetric file that can be archived and processed later. The transvaginal 3D ultrasound allows simultaneous visualisation of a given organ in three perpendicular planes for accurate measurements of dimensions and volumes, while simultaneously viewing the external contours of the examined structure. The saved volumetric image can be rotated and viewed in all planes. In reproductive medicine, 3D ultrasonography has many potential applications, including assessment of congenital and acquired uterine defects, ovarian patency, ovarian observation and their response to ovulation stimulation, as well as the evaluation of endometrial receptivity. In addition, the three-dimensional Power Doppler angiography allows you to assess the flow volume in the ovary and endometrium.
Indications for ultrasound examination:
- Periodic assessment of the reproductive system (prophylactically every 2 years)
- Diagnostics of developmental disorders of the reproductive system
- Diagnostics of uterine pathology, appendages
- Cancer diagnostics
- Early pregnancy diagnostics
- Diagnostics of gynaecological endocrinological disorders
Computer Assisted Semen Analysis (CASA)
Semen analysis is a basic component of infertility diagnostics. The parameters taken into account for the assessment of semen in accordance with the guidelines of the World Health Organization (along with the 2010 reference values) are:
Reference values for semen analysis according to WHO 2010 guidelines:
Semen volume: | <= | 1,5ml |
pH: | >= | 7,2 |
Liquefying time: | < | 60 minutes |
Semen agglutination and aggregation: | none |
Sperm count*:
| per 1 ml (concentration, density) | >= 15 mln/ml (>= 15 * 106 / ml) |
| in ejaculation (total) | >= 39 mln / ejaculation (>= 39 * 106 / ejaculation) |
Sperm Motility:
| General (progressive + non-progressive motility) | >= | 40% |
| Progressive motility | >= | 32% |
| Sperm life | >= | 58% |
| Sperm morfology | >= | 4% |
| Leukocytes (peroxidase-positive) | < 1 mln/ml (< 1 * 106 / ml) | |
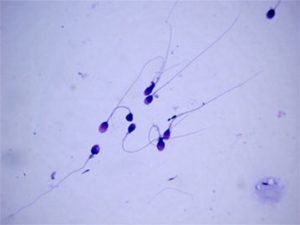
Routine semen analysis was performed using an optical microscope. Unfortunately, this is a subjective assessment, and though it does not make it difficult to assess the sperm count, there may often be deviations when assessing sperm motility. The inability to objectively analyse the percentage of progressive sperm has resulted in the development of computer assisted semen analysis (CASA). This system consists of combining phase contrast microscopy with a camera, computer and specialised software, which allows to view subsequent sperm positions at a frequency of 5-60 images per second, and transfer the saved images into digital form. It is subjected to a computer analysis allowing for accurate and objective analysis of the motility trajectory of each sperm.
.
Female hormonal teksts
Hormonal tests should be performed in cases of suspected endocrinopathy, and in all patients starting IVF treatment. They should include: folliculotropin (FSH), luteinizing hormone (LH), estradiol, prolactin (in specific cases), and progesterone in the middle of the second phase of cycle.
Chronic anovulation is diagnosed when the concentration of progesterone, measured at least three times in the middle of the luteal phase, is less than 3 ng/ml. To evaluate the ovarian reserve, it is important to determine the FSH level during days 2-5 of the cycle.
If it is elevated, diagnostics can be expanded to include the AMH (Anti-Müllerian hormone) and inhibin B tests. It is not currently recommended to routinely test prolactin levels in patients with regular menstrual periods. However, it should be performed if the menstrual cycle is irregular. Prolactin concentrations in excess of 200 μg/l (9 nmol/l) are an indication for further diagnostics due to the risk of pituitary adenoma.

Hormonal tests are also very useful for assessing the presence and quality of ovulation. It is highly probable that ovulation cycles are present in a woman who menstruates regularly every 21 to 35 days. This is confirmed by an ultrasonographic examination showing the presence of a growing follicle reaching a diameter of 16-22 mm in the periovulatory phase, and determining oestradiol concentrations in the periovulatory phase ( 150 – 300pg/ml), as well as serum progesterone seven days before expected menstruation (above 10ng/ml).
Endocrine diagnostic tests are also useful in determining indications for, plans and monitoring of treatment. FSH values above 10-12 mIU/ml in women indicate a reduced ovarian reserve and a high probability of a poor response to stimulation, while its values above 20mIU/ml indicate ovarian insufficiency. Additional determination of AMH and inhibin B values allows for more accurate evaluation of reproductive potential, but also to optimise the work of medications used for induction of ovulation, and reduces the rate of failed stimulations and complications. This mainly concerns the stimulation and induction of ovulation in patients undergoing medically assisted reproduction.
Male hormonal tests

The basic indications for hormone evaluation are azoospermia (lack of sperm in the ejaculate) and oligozoospermia: <5 million sperm in 1 ml of semen. The basic diagnostics should include the measurement of serum FSH and serum testosterone levels. For hypoandrogenic symptoms, the level of inhibins, LH, estradiol and prolactin should be tested in addition to FSH levels.
Elevated FSH values indicate spermatogenic disorders. This is not a clear-cut study: elevated FSH levels have been observed with spermatogenesis, and normal values were present with spermatogenic disorders. If azoospermia is detected in the semen sample and the andrological examination is normal, a biopsy of the testes is required. Histopathological examination of the content of the testis is aimed at finding the preserved course of spermatogenesis and the presence of spermatozoa.
The best predictor of the presence of spermatozoa in the testicles or epididymis is the serum FSH concentration test. If FSH> 15 mjm./ml, the chance of their presence in the tested content is <20%, if FSH is > 25 mjm./ml it is close to zero. Therefore, the serum FSH test can be considered as one of the stages of differential diagnosis of azoospermia (due to obstruction of the seminal tract) resulting in the presence of normal FSH values. With non-obstructive azoospermia, FSH values may be elevated or normal, and testosterone levels may be lower. Reduced FSH, LH and testosterone levels are observed in hypogonadotropic hypogonadism.
Hysteroscopy
It is a minimally invasive method of gynaecological endoscopy. According to the scope of the examination and indications for its implementation, either diagnostic or surgical hysteroscopy may be performed.
 Diagnostic hysteroscopy – is a particularly important test in the diagnosis of uterine endometrial disorders. By using a hysteroscope, a special optical device equipped with an optical fibre, it is possible to accurately assess the cervical canal and the uterine cavity.
Diagnostic hysteroscopy – is a particularly important test in the diagnosis of uterine endometrial disorders. By using a hysteroscope, a special optical device equipped with an optical fibre, it is possible to accurately assess the cervical canal and the uterine cavity.
When examining the uterine cavity, the focus is on the following:
- Presence of abnormalities in the cavity structure – diagnosis of uterine defects (bicornuate uterus, uterine septum)
- Presence of pathology within the endometrium – presence of endometrial polyps, intrauterine adhesions, endometrial hyperplasia
- Presence of submucosal fibroids
- Reactive processes of the fallopian tubes
Indications for diagnostic hysteroscopy include infertility, repeated failed IVF treatment, miscarriages, and abnormal uterine bleeding. Diagnostic hysteroscopy is usually performed in the first half of the cycle (days 7-13 of the cycle) by inserting a thin hysteroscope (4-5 mm) through the vagina and cervix into the uterine cavity. Thanks to the presence of the camera it is possible to record the procedure and to back the examination results with photographic documentation. Diagnostic hysteroscopy can be performed without anaesthesia because, due to the very small diameter of the hysteroscope, it is not a painful procedure. However, if the patient experiences discomfort or pain, a short-term intravenous anaesthetic may be administered by the anaesthetist.
Surgical hysteroscopy – is used to treat disorders detected during diagnostic hysteroscopy. The hysteroscope is equipped with a tube through which surgical tools are inserted to remove the lesions – endometrial polyps, fibroids, adhesions, septum or hyperplasia. The following measures must be taken prior to undergoing the surgical hysteroscopy procedure:
- Patient should be fasting (for at least 6 hours)
- Patient should be vaccinated against hepatitis B
- Current lab test results:
- Blood type
- CBC
- Coagulation tests APTT and PT
- Serological tests for chlamydia
- HIV, HCV, HBsAg, VDRL, anti-HCV (in the past 6 months)
- Cytology
- Degree of purity
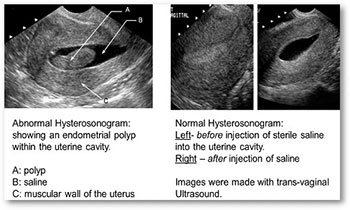
Sonohysterosalpinography
It is a test to diagnose abnormalities of:
- Structure of the uterus (submucosal fibroids, congenital defects of the uterus, septum)
- Endometrium (endometrial polyps, intrauterine adhesions, endometrial hyperplasia)
- Assessment of tubal patency
The procedure is performed on a gynaecological chair and requires the insertion of a speculum. After disinfecting the cervix, a sterile balloon catheter is inserted into the cervical canal, filled with fluid in order to secure it. Next, a saline solution or special substance is administered into the catheter. Liquid fills the uterine cavity. While the liquid is being administered a transvaginal ultrasound is performed. The shape and size of the uterine cavity, and the presence of pathological endometrial bulges are evaluated. The patency of the fallopian tubes is checked by evaluating the passage of fluid from the uterine cavity through the fallopian tubes to the abdominal cavity. After the test, the catheter is removed from the uterus and the patient can return to daily activities. The treatment usually lasts no longer than 30 minutes.
Preparing for the test:
- The test is performed in the first week after menstruation (after bleeding and spotting have completely stopped)
- Previously performed detailed gynaecological ultrasound examination (preferably with documentation)
- Evaluation of vaginal purity (vaginal microbiological smear)
- Current cytology (performed within one year)
Treatment for men with a spinal cord injury
There are situations where the problem lies with the man and is due to inability to obtain semen. This is often the case in men who have suffered a permanent spinal cord injury in the past and are now wheelchair-bound. In such cases, the semen can be obtained surgically through a biopsy of the epididymis or testes (MESA/TESA). In cases where the obtained semen shows normal values in terms of number and quality of sperm, insemination is sufficient. Unfortunately, it often does not meet the required norm, having very short sperm viability and a significant percentage of dead sperm, which is an indication for ICSI IVF treatment. As in other cases, once obtained, the reproductive material of a man can be frozen and used repeatedly.

